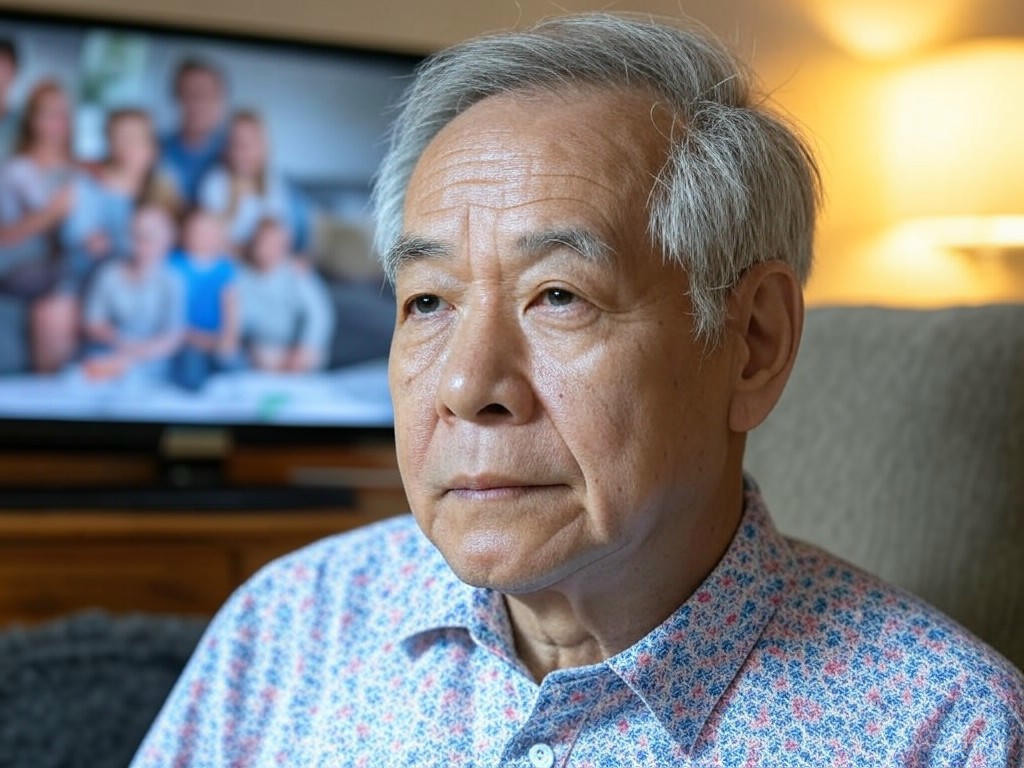
Could a Childhood Virus Pave the Way for Alzheimer’s Later in Life?
A startling connection between a common childhood virus and Alzheimer’s disease has resurfaced in scientific discussions, raising questions about long-term health impacts. Decades-old research, first published in the early 1990s, pointed to a potential link between the herpes simplex virus type 1 (HSV-1)—often responsible for cold sores—and the development of Alzheimer’s in later years. While the findings initially sparked curiosity, they were met with skepticism. Now, as researchers revisit this correlation, the medical community is reevaluating its significance and what it could mean for future prevention strategies.
HSV-1 is a virus many of us encounter in childhood, often through harmless skin-to-skin contact. It’s estimated that over half the global population carries this virus, which lies dormant in nerve cells for years, occasionally flaring up as cold sores during times of stress or illness. The original study suggested that in some individuals, this virus might travel to the brain, triggering inflammation and contributing to the buildup of amyloid plaques—a hallmark of Alzheimer’s disease. This theory posits that the virus could act as a silent catalyst, setting the stage for cognitive decline decades after initial exposure. While the idea was groundbreaking, it lacked conclusive evidence at the time, leaving many experts unconvinced of its relevance.
Fast forward to today, and advancements in neuroscience have allowed scientists to take a closer look at this potential connection. Modern studies using sophisticated imaging and genetic analysis have reignited interest in how viral infections might influence neurodegenerative conditions. Some researchers argue that HSV-1 could exacerbate brain inflammation, a known risk factor for Alzheimer’s, especially in those with genetic predispositions. Others caution against overinterpreting the data, emphasizing that correlation does not equal causation. After all, millions carry HSV-1 without ever developing Alzheimer’s, suggesting other environmental or lifestyle factors likely play a larger role. Doctors also point out that while the virus might be a contributing factor, it’s far from the sole cause of the disease.
The debate continues to unfold, with experts divided on how much weight to give this theory. For the average person, the takeaway isn’t to panic about a childhood cold sore but to stay informed about brain health. Neurologists recommend focusing on well-established protective measures—maintaining a healthy diet, staying physically active, and managing stress—to reduce Alzheimer’s risk. Meanwhile, ongoing research aims to clarify whether antiviral treatments could one day mitigate any potential effects of HSV-1 on the brain. Until then, the medical community urges caution in drawing firm conclusions from these early findings.
As science progresses, the relationship between common viruses and complex diseases like Alzheimer’s may become clearer. For now, this intriguing link serves as a reminder of how interconnected our early health experiences can be with our later years. It’s a call to prioritize overall wellness, knowing that even small steps today might safeguard our cognitive future tomorrow.